
Acute encephalitis syndrome caused by Orientia tsutsugamushi
Introduction
Acute encephalitis syndrome (AES) secondary to scrub typhus is a rare life-threatening medical emergency. The severity varies from mild meningitis to meningoencephalitis. Clinicians often lack awareness of this presentation of scrub typhus, which leads to difficulty and delay in diagnosis, causing significant morbidity and mortality. We present a case of AES secondary to scrub typhus.
Case presentation
The patient was a 50-year-old man working as an entomologist without any previously documented systemic diseases. He was brought to our emergency department (ED) by an ambulance presenting with generalized tonic-clonic seizure (GTC) and alteration of consciousness. According to the patient’s wife, he was healthy 8 days prior to the ED arrival when he developed intermittent fever, productive cough, and headache, and 6 days prior to the ED arrival, developed persistent hiccup, retches, and anorexia. One day prior to the ED arrival, weakness, disorientation, and bizarre behavior were noted.
An episode of GTC occurred with urine and stool incontinence, and he became unresponsive. Glasgow Coma Scale score was E4V2M4. There was no recent history of trauma, weight loss, syncope, vomiting, choking, sore throat, muscle soreness, chest pain, abdominal pain, leg edema, oliguria, dysuria, tarry stool passage, hematuria, animal scratching, special-dye intake in diet, illicit drug usage, special contact, or overseas travel.
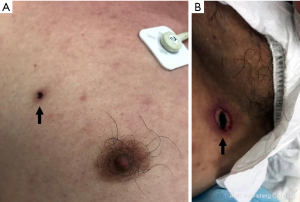
At ED, a physical examination revealed fever (body temperature: 39.4 °C), tachycardia (pulse rate: 135 beats per minute), hypotension (systolic/diastolic blood pressure: 77/61 mmHg), skin rashes over the trunk (Figure 1), disorientation, and two eschar lesions over his right chest wall (Figure 2A) and thigh (Figure 2B), but no focal neurologic deficits. Endotracheal intubation was performed for airway protection. Intravenous fluid resuscitation was performed, and antipyretic agent propacetamol 1 gm was intravenously administrated.
Laboratory data showed leukocytosis [white blood cell (WBC) count: 21,600/µL, band neutrophils: 2%, segmented neutrophils: 94%, lymphocytes: 2%, monocytes: 2%], thrombocytopenia (platelet count: 75,000/µL), hyponatremia, lactic acidosis, renal impairment, mildly prolonged prothrombin time (international normalized ratio: 1.25), hyperglycemia (blood glucose level: 676 mg/dL), hyperosmolality (osmolality: 319 mOsm/kg), elevated ammonia (blood ammonia: 88 µg/dL), and elevated aspartate aminotransferase (AST) (blood AST: 114 IU/L). Cranial computed tomography (CT) demonstrated no obvious signs of intracranial hemorrhage. A chest X-ray scan revealed diffuse ground-glass opacities in both lung fields. With a tentative diagnosis of central nervous system (CNS) infection, lumbar puncture was performed smoothly. Cerebrospinal fluid (CSF) study revealed positive Pandy’s test; WBC: 4/mm3; glucose: 273 mg/dL; total protein: 71 mg/dL; chloride: 111 mEq/L; and lactate dehydrogenase (LDH): 21 IU/L. Doxycycline (100 mg) and high-dose ceftriaxone (2 gm) were administered. After the emergent management, he was admitted to our medical intensive care unit (MICU) for further treatment. He was extubated and transferred to MICU 3 days after the ED arrival. On the 4th day of admission, real-time polymerase chain reaction test was positive for tsutsugamushi. Finally, he recovered and was discharged 9 days later.
Discussion
Scrub typhus is an acute mite-borne febrile illness caused by Orientia tsutsugamushi. The incubation period of scrub typhus is 5 to 14 days. People who perform outdoor activities such as farming and fishing in a jungle are most frequently affected (1,2). Patients can present with non-specific flu-like symptoms, such as headache, myalgia, cough, nausea, and vomiting. The most common symptoms are fever and headache. Some of them have an eschar at the bite location, which is mostly the front of the body. Men and women haves some differences in the bite location. The common locations in men are below the umbilicus within 30 cm, lower extremities, and anterior chest, while in women are anterior chest, and head and neck regions. In addition to the sites mentioned above, children commonly find eschar in the axillae (3). Severe multi-organ complications can arises, resulting in tubulointerstitial nephritis (TIN) with acute renal failure (ARF), interstitial pneumonitis with adult respiratory distress syndrome (ARDS), and disseminated intravascular coagulation (DIC) (4,5).
CNS involvement is a known complication of scrub typhus, and its common symptoms include seizures, altered sensorium, and vomiting (6). Occasionally, although CNS is involved, dCSF is clear in appearance (6). Usually, the presence of fever and eschars support the diagnosis. Scrub typhus shows a good response to doxycycline, which is recommended for the treatment (2).
Our patient had probably exposed himself to an infested ground, as eschars were found on his anterior chest wall and right thigh. CSF study revealed no definite infection type. His condition resolved rapidly after doxycycline administration. In a scrub typhus emergency, acute febrile illness with CNS symptoms require timely diagnosis and treatment to prevent mortality and disease sequelae. This case highlights the need for a high degree of suspicion for AES secondary to scrub typhus to diagnose it early and to start specific treatment immediately. Patients usually recover soon with a good outcome.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: WHC serves as an Editor-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jamil MD, Hussain M, Lyngdoh M, et al. Scrub typhus meningoencephalitis, a diagnostic challenge for clinicians: A hospital based study from North-East India. J Neurosci Rural Pract 2015;6:488-93. [Crossref] [PubMed]
- Chakraborty S, Sarma N. Scrub Typhus: An Emerging Threat. Indian J Dermatol 2017;62:478-85. [PubMed]
- Xu G, Walker DH, Jupiter D, et al. A review of the global epidemiology of scrub typhus. PLoS Negl Trop Dis 2017;11:e0006062 [Crossref] [PubMed]
- Kar A, Dhanaraj M, Dedeepiya D, et al. Acute encephalitis syndrome following scrub typhus infection. Indian J Crit Care Med 2014;18:453-5. [Crossref] [PubMed]
- Chi WC, Huang JJ, Sung JM, et al. Scrub typhus associated with multiorgan failure: a case report. Scand J Infect Dis 1997;29:634-5. [Crossref] [PubMed]
- Mittal M, Thangaraj JWV, Rose W, et al. Scrub Typhus as a Cause of Acute Encephalitis Syndrome, Gorakhpur, Uttar Pradesh, India. Emerg Infect Dis 2017;23:1414-16. [Crossref] [PubMed]
Cite this article as: Wang CY, Chang WH, Su YJ. Acute encephalitis syndrome caused by Orientia tsutsugamushi. Health Technol 2019;3:5.



