Explore patient-specific needs for mHealth solutions in Taiwan: a mixed study
Introduction
In today’s fast-paced world, increased ownership of smartphones and tablets has led to rapid growth in the development of mHealth applications (apps). As a result, health providers now use innovative information technologies to deliver more convenient, safer, accessible, and affordable quality of care (1).
There are more than 97,000 mobile apps related to health available on the main app stores worldwide. In 2017, the estimated number of mHealth applications downloaded was 3.7 billion. The digital health market is expected to reach 206 billion USD by 2020. In addition, 52% of smartphone users collect health-related information on their phones (2). Despite mHealth’s popularity and potential, most projects implementing information technology within the field of health care during the past decade, have been unsuccessful with approximately 70% of projects being abandoned or failing (3). Health information technology will not achieve its goals unless it provides healthcare workers and patients with the ability of make decisions and solve problems (3,4). Knowing how users think and behave will help to engage with and motivate patients, which could inspire more efficient and effective health control for the target group (5,6).
Methods
Procedure and participants
This quantitative and qualitative study to explores patients’ experiences of mHealth technology. The Human Research Ethics Committee of Mackay Memorial Hospital waived the requirement to obtain informed consent for the study. In accordance with this approval, participants provided signed informed consent for the interviews.
The participants were patients of the MacKay Memorial Hospital, Taipei Taiwan. The interviews were conducted on October 13, 15, and 16, 2017, in Mandarin. The survey included participants in a broad age range in order to combine the experiences of the tech-savvy younger generation with those of the elderly generation. We categorize the mobile medicine platform into three age groups, namely, 29 and under, 30 to 59, and 60 and over. A total of 220 participants enrolled in the survey, comprising 106 males and 114 females.
Measures
Semi-structured questionnaires provided participants with the freedom to elaborate on the interview guide. The out of the 220 patients were interviewed for between 10 and 15 minutes. These interviews were digitally recorded and transcribed verbatim.
Results
Description of participants
The 220 randomly selected patients included 106 males and 114 females, accounting for 48.2% and 51.8%, respectively, of the total number of subjects. The most common age bracket is 30–59 years of age (67.3%). The age group of 29 and under includes 53 participants (24.1%), and the age group of 60 and older includes 19 participants (8.6%). Further participant demographics are provided in Table 1.
Table 1
| Age (years) | Male, n (%) | Female, n (%) | Total, n (%) |
|---|---|---|---|
| Under 19 | 4 (1.8) | 1 (0.5) | 5 (2.3) |
| 20–29 | 23 (10.5) | 25 (11.4) | 48 (21.8) |
| 30–39 | 38 (17.3) | 34 (15.5) | 72 (32.7) |
| 40–49 | 14 (6.4) | 27 (12.3) | 41 (18.6) |
| 50–59 | 13 (5.9) | 22 (10.0) | 35 (15.9) |
| 60–69 | 12 (5.5) | 4 (1.8) | 16 (7.3) |
| Over 70 | 2 (0.9) | 1 (0.5) | 3 (1.4) |
| Total | 106 (48.2) | 114 (51.8) | 220 (100.0) |
Sample characteristics
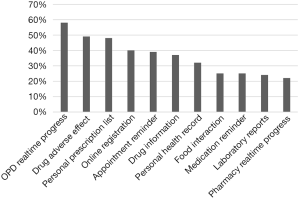
The top three features preferred by participants (in order) are, real-time outpatient progress (58%), adverse effects of medicine (49%), and personal prescription lists and electric medical records (48%) (Figure 1). The willingness to use a mobile application provided by the hospital that offers the requested features and functions is as follows: 36.4% absolutely and 46.8% probably, for own demand, and 34.5% absolutely and 40.5% probably for their family (Table 2).
Table 2
| Level of willingness | Self-employment (%) | For family need (%) |
|---|---|---|
| Definitely | 36.4 | 34.5 |
| Possible | 46.8 | 40.5 |
| Neutral | 7.7 | 6.8 |
| Probably not | 5.9 | 11.8 |
| Absolutely not | 3.2 | 6.4 |
Age and digital capability
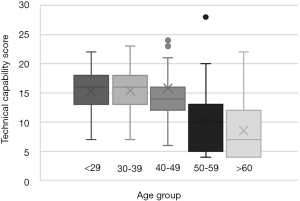
Different age groups share different digital capabilities. We assign scores (minimum 1 and maximum 7) to each of the four questions in the questionnaire, which are then totaled (minimum 4 and maximum 28) to represent the digital capability of a person. The questions are related to the years using a smartphone, total number of apps downloaded, number of apps used per day, and average hours spent per day on a smartphone browsing the internet and using apps. A score of 14 and above is considered competent. In terms of digital capability, which was found to be significantly better in people below the age of 50 (Figure 2).
Emerging themes by respondents
The five major themes related to the influence of mHealth technology, as indicated by respondents are as follows: notify patient and minimize prescription wastes; record daily patient medication adherence; convenient medication information on the mobile application; big data analyses on the data collected; and interaction between patients and healthcare professionals, as well as family and other patients.
“I like to check online reviews of doctors before making an appointment, and always check medication information. I’d love to use an mHealth mobile application for my family.” —22-year-old male visiting the dermatology outpatient department (OPD) for a skin rash.
“I believe in everything that doctor tell me. I don’t need further drug information.” —22-year-old female; OPD follow-up for minor discomfort.
“I always take medicine till total recovery. I pay attention to the possible medical adverse effect. Sometimes, I ask for an opinion on medical issues from my sister, who is a doctor. I need to remind older family members to take medicine.” —26-year-old male; OPD follow-up for more prescription medication.
“I have experience of drug allergy before. I have used several mobile applications provided by other hospitals for my parents to save time. I am eager to obtain more complete and integrated medical information for my family and myself.” —40-year-old female; dermatology follow-up.
“I like to check for medical information and information on health supplements. I seek a doctor’s opinion.” —42-year-old male; regular ophthalmology follow-up.
“I am concerned about the quality and effect of prescribed medicine. Personal information safety is important to me. Parents need my accompany for every hospital visit.” —45-year-old female; rheumatology follow-up every 3 months.
“I feel like nothing I can do to obtain better quality of care. I would like to pay more for better drugs.” —50-year-old female with hypertension.
“I feel frustrated that I am not able to acquire better medical care just because I am an ordinary person. I am willing to pay more for better drugs.” —65-year-old female with hypertension and regular follow-ups by a family physician.
“I enter all prescription information to make a record, which I save on my smartphone. I am concerned about the pharmaceutical manufacturer and the ingredients of medicine. I am upset that I did not obtain enough pharmaceutical information from the pharmacist.” —70-year-old male visiting ophthalmology.
“I believe everything I am told by the doctor. I don’t check for medical information myself, and am not familiar with smartphones. I didn’t tell my doctor recently that I felt dizzy during the day’s appointment.” —70-year-old male with underlying cardiovascular chronic disease; return for follow-up and drug prescription renewal.
Discussion
Principle findings
Outpatient real-time progress is the most desired feature presented in our study. Medical professionals emphasized more on physician’s time in the past. However, this is no longer valid in today’s consumer-oriented world. Waiting time for patient is not only factor that affects patient satisfaction but it is one of the indexes to evaluate the quality of outpatient services (7-9). The real-time progress provided by outpatient management software showed reduction of patient waiting times and, consequently, improves patients’ satisfaction (10).
Drug adverse effects (49%), personal prescription records (48%), basic drug information (37%), and medication reminders (25%) occupy 4 of the top 10 requested features. Medication use is one of the most common health-related behaviors that patients perform on a daily basis to manage their health, However, it is also often one of the most difficult, because it places demands on patients’ memory and organization and planning skills (11). Although there were hundreds of mobile applications available from app stores to help consumers manage their outpatient medication use, there are also many complaints and concerns related to technical difficulties, the absence of desired features, and data safety. Thus, greater effort should be made to improve the design, content, and features of such applications from a patient perspective (12).
Interactions with social support
In the past, doctors communicated with patients by means of clinic appointments. Patients and their families need to be collaborative partners in their healthcare and more engaged in their healthcare decisions (13). Using mobile technology, healthcare providers can extend their services by providing a suitable environment in which to make healthcare services accessible anywhere and at any time (14). This should lead to better decisions. As illustrated in this study, people are motivated to adopt mobile applications for their family’s healthcare. Mobile health applications that make family engagement possible will allow patients, families, their representatives, and health professionals working in active partnerships at various levels across the healthcare system to improve health and healthcare.
Awareness, motivation, and capability
Our interviews showed how patients from different age groups express their needs related to a mobile application to assist them in their daily health management. This study revealed the younger generation group tends to have lower awareness and motivation but with higher digital capability in adopting mHealth technologies. However, when a highly capable group becomes motivated, like being pregnant, being a novice parent, having first stroke event, or suffering from some chronic health condition, they will efficiently utilize the technology. In contrast, the elderly generation often struggles to adopt these technologies, despite feeling motivated to do so. A study showed the most often mentioned barriers from the elderly generation was complexity (15). Several studies have shown the potential of mobile health technology in terms of improving the health of older adults (16-21). Thus, incorporating novel ideas that empower older adults and their caregivers to manage their own conditions and to foster communications within the circle of care should be urged (22-26). Future mHealth design should focus on barriers related to complexity by increasing the ease of use or by moving the target to caregivers in order to facilitate further adoption (27).
Conclusions
Mobile technology is changing the way in healthcare delivery and patient-physician interactions. In terms of the values provided to patients, the benefits include medication reminders, shorter waits for appointments, timely and personal clinician interactions, convenient access to trustworthy health information, obtaining information from peers, and social support. Nevertheless, the include concerns over data privacy and leakages, information inaccuracy, and a lack of regulation and approval. A better understanding of consumer experiences and expectations will enable the design of a mobile platform that delivers helpful information and interactive education, an efficient workflow, and proactive tracking, including various types of feedbacks for different generations and for differing levels of motivation.
Acknowledgments
The authors acknowledge the Biomedical Development, Innovation and Incubation Center, Mackay Memorial Hospital, who helped the administrative process.
Funding: This work was supported by the joint research project by MacKay Memorial Hospital and HTC Corporation, Taiwan.
Footnote
Conflicts of Interest: WHC serves as an Editor-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Human Research Ethics Committee of Mackay Memorial Hospital (No. 18MMHIS016e). The ethics committee waived the requirement to obtain informed consent for the study. In accordance with this approval, participants provided signed informed consent for the interviews.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T 2014;39:356-64. [PubMed]
- Mag HM. Is mobile healthcare the future? Health Management Technology 2017. Available online: https://www.healthmgttech.com/mobile-healthcare-future
- Kaplan B, Harris-Salamone KD. Health IT success and failure: recommendations from literature and an AMIA workshop. J Am Med Inform Assoc 2009;16:291-9. [Crossref] [PubMed]
- Williams J. The value of mobile apps in health care. Healthc Financ Manage 2012;66:96-101. [PubMed]
- Singh K, Drouin K, Newmark LP, et al. Developing a Framework for Evaluating the Patient Engagement, Quality, and Safety of Mobile Health Applications. Issue Brief (Commonw Fund) 2016;5:1-11. [PubMed]
- Greene J, Hibbard JH, Sacks R, et al. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood) 2015;34:431-7. [Crossref] [PubMed]
- Sibbel R, Urban C. Agent-Based Modeling and Simulation for Hospital Management. In: Saam NJ, Schmidt B. editors. Cooperative Agents: Applications in the Social Sciences. Dordrecht: Springer Netherlands, 2001:183-202.
- Mohebbifar R, Hasanpoor E, Mohseni M, et al. Outpatient waiting time in health services and teaching hospitals: a case study in Iran. Glob J Health Sci 2013;6:172-80. [Crossref] [PubMed]
- Bleustein C, Rothschild DB, Valen A, et al. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care 2014;20:393-400. [PubMed]
- Almomani I, AlSarheed A. Enhancing outpatient clinics management software by reducing patients' waiting time. J Infect Public Health 2016;9:734-43. [Crossref] [PubMed]
- Bailey SC, Oramasionwu CU, Wolf MS. Rethinking adherence: a health literacy-informed model of medication self-management. J Health Commun 2013;18:20-30. [Crossref] [PubMed]
- Bailey SC, Belter LT, Pandit AU, et al. The availability, functionality, and quality of mobile applications supporting medication self-management. J Am Med Inform Assoc 2014;21:542-6. [Crossref] [PubMed]
- Skiba DJ. Digital taxonomy: evaluating and creating. Nurs Educ Perspect 2013;34:428-9. [PubMed]
- Anshari M, Almunawar MN. Mobile Health (mHealth) Services and Online Health Educators. Biomed Inform Insights 2016;8:19-27. [Crossref] [PubMed]
- Kruse CS, Mileski M, Moreno J. Mobile health solutions for the aging population: A systematic narrative analysis. J Telemed Telecare 2017;23:439-51. [Crossref] [PubMed]
- Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care 2011;34:308-13. [Crossref] [PubMed]
- Durso SC, Wendel I, Letzt AM, et al. Older adults using cellular telephones for diabetes management: a pilot study. Medsurg Nurs 2003;12:313-7. [PubMed]
- Larsen ME, Rowntree J, Young AM, et al. Chemotherapy side-effect management using mobile phones. Conf Proc IEEE Eng Med Biol Soc 2008;2008:5152-5.
- Scherr D, Kastner P, Kollmann A, et al. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res 2009;11:e34 [Crossref] [PubMed]
- Liu WT, Wang CH, Lin HC, et al. Efficacy of a cell phone-based exercise programme for COPD. Eur Respir J 2008;32:651-9. [Crossref] [PubMed]
- McCall K, Keen J, Farrer K, et al. Perceptions of the use of a remote monitoring system in patients receiving palliative care at home. Int J Palliat Nurs 2008;14:426-31. [Crossref] [PubMed]
- Matthew-Maich N, Harris L, Ploeg J, et al. Designing, Implementing, and Evaluating Mobile Health Technologies for Managing Chronic Conditions in Older Adults: A Scoping Review. JMIR Mhealth Uhealth 2016;4:e29 [Crossref] [PubMed]
- Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood) 2014;33:194-9. [Crossref] [PubMed]
- Willmer M. How nursing leadership and management interventions could facilitate the effective use of ICT by student nurses. J Nurs Manag 2007;15:207-13. [Crossref] [PubMed]
- Kennedy A, Rogers A, Bowen R, et al. Implementing, embedding and integrating self-management support tools for people with long-term conditions in primary care nursing: a qualitative study. Int J Nurs Stud 2014;51:1103-13. [Crossref] [PubMed]
- Kennedy A, Bower P, Reeves D, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346:f2882. [Crossref] [PubMed]
- Joe J, Demiris G. Older adults and mobile phones for health: a review. J Biomed Inform 2013;46:947-54. [Crossref] [PubMed]
Cite this article as: Huang ST, Chuang HY, Chang WH, Huang MY. Explore patient-specific needs for mHealth solutions in Taiwan: a mixed study. Health Technol 2018;2:1.