The potential risk of sick building syndrome of the emergency department areas in a medical center in Taiwan
Introduction
Indoor air pollution fits within the risk transition framework (1), in which the modern risks from building materials emerge and the traditional risks of household fuel combustion subside. It has always been a problem in today’s modern society, and there is no exception in the emergency department (ED). In recent years, the incidence of respiratory symptoms due to air pollution is higher in the more advanced countries. Therefore, environmental factors are considered to be one of the causes impacting the increase in the incidence of respiratory disease (2). Among environmental factors, it can be divided into allergic factors and non-allergic factors. Allergic factors triggering of acute respiratory disease include dust (3), cockroaches, mold, and etc. On the other hand, non-allergic factors found in hospitals, such as dirty and polluted air, will impact work efficiency of healthcare staffs and cause diseases; even some severe acute respiratory diseases are prone to outbreaks in hospitals. The causative microorganisms often transmit and infect humans/medical staff through air, which could then be further passed on to patients and even worsening the patient’s condition. These are all major causes of nosocomial infections. To medical staffs, how to being familiar with the medical working environment, and prevent the threat of nosocomial infection, is a very important issue. Poor indoor ventilation, or excessive generation of tiny particles, can cause substantial discomfort on the human body. Negative effects of unhealthy indoor environment are often accompanied by general symptoms such as headache and inattention. Poor indoor air quality can reduce the performance of office work by 6–9% (4). An approximately linear relationship between the percentage dissatisfied with indoor air quality (from 20–70%) and the measured decrement in performance was observed (5). Therefore, how to improve air quality in ER has become an important issue.
Methods
This study is designed to monitor the air quality in ten locations in the Department of Emergency Medicine of the Mackay Memorial Hospital, which is a medical center that has nearly 200,000 emergency patient visits per year. The Taipei District covers about 140,000 emergency patient visits per year. The ER of Mackay Memorial Hospital, Taipei District, covers an area of approximately 1,500 square meters, which can simultaneously accommodate approximately 160 patients.
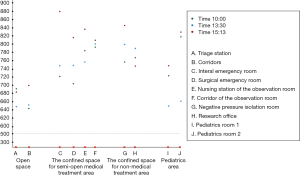
The emergency areas were classified into four types and assessed according to whether it was confined or not, and whether medical treatment was performed or not, as follows: (I) open space—triage station, corridors; (II) confined space for semi-open medical treatment area—surgical ER, internal medicine ER, nursing station of the observation room, and corridor of the observation room; (III) confined space for non-medical treatment area—the negative pressure isolation room and research office; and (IV) the pediatric areas—pediatrics rooms one and two. The data collected were analyzed and compared. At least 12 physicians and 24 nurses participated at each session. The ER area was jointly organized by the new building (approximately 1,254 square meters) and the old building (approximately 231 square meters). The nursing station and corridor of the observation room, as well as the research office, are in the 50-year-old buildings, while the other areas are in new buildings constructed within 20 years.
Indoor air quality monitoring equipment (Figure 1), provided by the National Taipei University of Technology, was used to perform non-continuous monitoring thrice during the e daytime in the Department of Emergency Medicine. These included a thermometer, oxygen, carbon dioxide (CO2), ozone, total volatile organic compounds, suspended particle matter of 10 micrometers or less (PM10), and formaldehyde.
The scheduled research measurement time was 15:13 pm on 4 October 2010, 10:00 am on 5 October 2010, and 13:30 pm on 5 October 2010. According to the Central Meteorological Bureau, the temperature and humidity were 25 °C and 70% on October 4th, and 24 °C and 59% on October 5th, respectively. The research monitoring was conducted at the ten monitoring locations and recorded based on the following standard procedures: first, all the monitoring instruments were placed on the test bench, calibrated and then started the measurement. Until the measurement figures showed stability, such data was then recorded.
Results
The monitoring results of this study showed that the concentration of oxygen in the ED was higher than the background value of the general environment (20.9%). The oxygen concentration of most places in ER exceeded 30%. The concentration of carbon dioxide we measured in almost the entire area of ER has reached over 700 ppm, which exceeded the recommended standard value (600 PPM). Particularly in the internal medical ER, the surgical ER as well as the negative pressure isolation room, these three areas were found to have exceptionally higher CO2 concentrations up to 800 ppm (P<0.05) (Tables 1-3). A highest value of formaldehyde (0.14 ppm) was detected in the corridor of the observation room. Our study also showed that in the air of observation room and the research office in ER, there was more measured formaldehyde at different time periods; especially it was up to 0.14 ppm in the midday period (13:30 pm). In addition, the research office and the nursing station of the observation room were detected with a higher concentration of ozone in all three of the scheduled monitoring periods; conversely, ozone concentrations were not detected during the morning and midday timeslots from the air at the triage station. The research also showed fewer volatile organic compounds (TVOC) in the triage station, research office and the corridors, whereas other areas of ER had relatively higher TVOC concentration exceeding 150 ppb (normal 100 ppb). The measured values of suspended particles (PM10) with size less than 10 microns were within normal range at all measured locations.
Table 1
| Locations | Parameters | ||||||
|---|---|---|---|---|---|---|---|
| Temperature (°C) | O2 (%) | CO2 (ppm) | O3 (ppb) | VOC (ppb) | PM10 (μm/m3) | Formaldehyde (ppm) | |
| Triage station | 26.9 | 30.3 | 646 | 0.00 | 104 | 39 | 0.05 |
| Surgical emergency room | 26.5 | 30.3 | 708 | 0.00 | 244 | 63 | 0.05 |
| Internal emergency room | 26.9 | 30.4 | 723 | 0.00 | 186 | 28 | 0.00 |
| Pediatrics room 1 | 26.8 | 30.3 | 724 | 0.00 | 647 | 21 | 0.06 |
| Pediatrics room 2 | 26.2 | 30.3 | 818 | 2.10 | 317 | 0 | 0.02 |
| Corridors | 24.4 | 30.3 | 687 | 3.70 | 145 | 22 | 0.08 |
| Negative pressure isolation room | 24.2 | 30.4 | 767 | 7.20 | 441 | 2 | 0.08 |
| Nursing station of the observation room | 23.1 | 30.5 | 782 | 14.90 | 521 | 93 | 0.10 |
| Corridor of the observation room | 23.7 | 30.5 | 789 | 4.10 | 264 | 10 | 0.10 |
| Research office | 26.7 | 30.3 | 758 | 6.70 | 235 | 8 | 0.05 |
VOC, volatile organic substance.
Table 2
| Locations | Parameters | ||||||
|---|---|---|---|---|---|---|---|
| Temperature (°C) | O2 (%) | CO2 (ppm) | O3 (ppb) | VOC (ppb) | PM10 (μm/m3) | Formaldehyde (ppm) | |
| Triage station | 26.7 | 30.3 | 650 | 0.00 | 166 | 0 | 0.02 |
| Surgical emergency room | 27.5 | 30.3 | 800 | 4.00 | 254 | 50 | 0.03 |
| Internal emergency room | 26.5 | 30.3 | 747 | 3.40 | 321 | 18 | 0.03 |
| Pediatrics room 1 | 26.2 | 30.3 | 653 | 4.90 | 469 | 23 | 0.02 |
| Pediatrics room 2 | 25.9 | 30.3 | 664 | 0.00 | 294 | 16 | 0.00 |
| Corridors | 25.7 | 30.3 | 644 | 0.00 | 106 | 27 | 0.08 |
| Negative pressure isolation room | 24.1 | 30.4 | 796 | 3.90 | 361 | 38 | 0.09 |
| Nursing station of the observation room | 24.9 | 30.4 | 757 | 3.30 | 326 | 26 | 0.07 |
| Corridor of the observation room | 23.7 | 30.4 | 783 | 0.00 | 217 | 6 | 0.14 |
| Research office | 23.3 | 30.3 | 788 | 5.60 | 187 | 5 | 0.12 |
VOC, volatile organic substance.
Table 3
| Locations | Parameters | ||||||
|---|---|---|---|---|---|---|---|
| Temperature (°C) | O2 (%) | CO2 (ppm) | O3 (ppb) | VOC (ppb) | PM10 (μm/m3) | Formaldehyde (ppm) | |
| Triage station | 26.8 | 20.9 | 694 | 5.3 | 193 | 61 | 0.02 |
| Surgical emergency room | 27.8 | 20.9 | 812 | 4.2 | 268 | 55 | 0.03 |
| Internal emergency room | 28.4 | 30.4 | 883 | 0.0 | 329 | 28 | 0.01 |
| Pediatrics room 1 | 28.5 | 30.4 | 751 | 0.2 | 255 | 29 | 0 |
| Pediatrics room 2 | 28.4 | 30.4 | 824 | 5.9 | 271 | 38 | 0 |
| Corridors | 28.4 | 30.4 | 682 | 12 | 364 | 37 | 0 |
| Negative pressure isolation room | 27.8 | 30.5 | 851 | 4.8 | 465 | 25 | 0 |
| Nursing station of the observation room | 28.4 | 30.5 | 836 | 8.6 | 483 | 47 | 0.06 |
| Corridor of the observation room | 28.5 | 30.5 | 809 | 7.6 | 608 | 24 | 0.1 |
| Research office | 28 | 30.4 | 741 | 6.1 | 431 | 21 | 0.1 |
VOC, volatile organic substance.
CO2 level is an important indicator in air-quality monitoring. According to the statistics we obtained in various areas of the ER, we drew a scatter plot (Figure 2). In addition to the research office, CO2 concentration in most areas in the afternoon was relatively higher than morning and noon time. There was no significant difference in average concentration of CO2 measured in the districts of ED at the three times slots during 1 day (740, 728, and 788 ppm; P>0.05) (Table 4). Comparing the average CO2 concentration in the open space with the confined space, the former had better air quality (667 vs. 785 ppm; P<0.05) (Table 5). Open space had a relatively lower accumulation of CO2, due to air circulation and absence of medical activity in this area. Therefore, the air quality was better in the semi-open medical treatment area than a confined space. Except for the research office, the CO2 concentration in the afternoon was highest in all districts (15:13) (Figure 2). The research office had poorest air quality at 13:30 in the afternoon; however, the air quality was better in the open area and the pediatric area at the same time. The confined space for semi-open medical treatment area had better air quality at 10:00 am in the morning.
Table 4
| Time | Maximum | Minimum | Average | SD |
|---|---|---|---|---|
| 10:00 | 646 | 818 | 740 | 52 |
| 13:30 | 644 | 800 | 728 | 67 |
| 15:13 | 682 | 883 | 788 | 68 |
SD, standard deviation.
Table 5
| Variable | Locations | P | |
|---|---|---|---|
| Confined space | Open space | ||
| Time | |||
| 10:00 | 750±41 | 666±29 | <0.05* |
| 13:30 | 771±24 | 647±4.2 | <0.05* |
| 15:13 | 835±34 | 688±8.4 | <0.05* |
| Average value | 785 | 667 | <0.05* |
*, P<0.05. Data were presented as mean ± SD. SD, standard deviation.
Discussion
The concentration of indoor air pollutants varies greatly depending on living habits. For example, in the RIOPA study (6), which was conducted in an US urban residential area, about 60% of the fine particulate matter (PM2.5) mass came from outdoor atmosphere, and 40% resulted from indoor activities. On the other hand, the study in urban industrial areas of Kocaeli City, Turkey showed that contribution of outdoor pollutant sources to indoor pollution was about 70%, making these sources the most significant for indoor heavy metal pollution, whereas other sources of indoor pollution included smoking and cooking activities (7). Other indoor activities also generated PM2.5 in the work environment. In the emergency medical environment, the air composition and concentration were influenced by the use of oxygen, volatile compounds, alcohol, and some other medical treatments, such as putting on a plaster cast.
Our study found that, compared with the environmental background values (20.9%), the oxygen concentration was much higher in the ER, which may be caused by the high utilization of oxygen. In our measurement results, it was found that the value of concentration of formaldehyde was slightly higher (>0.12 ppm) in the space with more compartments, such as the area around the observation room and the research office. The research office had the highest concentration of ozone. The reason may be that the laser printers work all day long and produce much more ozone substances into the environment. Contrarily, the medical treatment room had poor air quality at 13:30 in this study due to more staffs working at that time. However, the air quality becomes better at 15:30 as working staffs decreases.
The ER is a high-risk and harsh environment. Although varying concentrations of CO2 were detected in different areas, the average value was greater than 700 ppm, which exceeds both the concentration of CO2 in the atmosphere and the EPA-recommended value of CO2 (600 ppm) in hospitals. Overall, the open space has less CO2 gas accumulation than confined space due to the relatively better air circulation and no medical behavior performed there. The monitoring data we collected from all the three timeslots showed that the concentration of CO2 was high. The CO2 concentration we measured was close to 800 ppm in the internal and surgical ER, as well as in the negative pressure isolation room. Except for the above areas, there were no significant differences between the remaining areas. What really affected the air monitoring data should be the people in the tested space at the time of the monitoring, including medical staffs, patients, and visitors. In addition, the humidity could be reduced due to regularly cleaning of the floor by cleaning works. The air quality of the open space was better than that of the confined space of the semi-open medical treatment area. This might be because people exhaled a great amount of CO2 in the ER, so that the amount of ventilation given by hospital air conditioner was insufficient to purify the air, resulting in confined space confinement (8,9). Another study showed that the frequent access to the tested space of wheelchairs or hospital beds also increased the number of suspended particles (10-12). We should reduce the number of people in the space or increase the ventilation of hospital air conditioner in order to improve CO2 indicators of ER in the future. Our study showed better air quality at 10:00 am, possibly because there was a lower number of patient visit during this period and relatively lowering CO2 accumulation. The sources of indoor CO2 were mainly from human breathing, smoking, and other burning activities (13). The concentration of indoor CO2 had a propensity to accumulate, due to high personnel density or inefficient ventilation efficiency (14). At the same time, the concentration of other pollutants was relatively increased. Therefore, CO2 is regarded as the most important chemical indicator of indoor air quality. Furthermore, it is an important indicator for assessing whether the indoor personnel density is too high and whether the ventilation efficiency is good. Carbon dioxide in the normal atmosphere is between 350 and 400 ppm, and it stimulates the respiratory center and cause dyspnea when it exceeds 400 ppm. High indoor CO2 concentrations in an office environment cause sleepiness during cognitive work (15). The accumulation of CO2 also significantly reduces decision-making performance (16), which is one of the most important ability of ER staffs. Previous studies have shown that architectural design was significantly associated with some symptoms, meaning that people feel uncomfortable in an environmentally poor building, a phenomenon known as “sick building syndrome (SBS)” (17). Symptoms of SBS include dizziness, headache, fatigue, dry throat, stinging eyes, wheezing, dizziness, nasal sensitivity, sneezing, nasal congestion, inability to concentrate, nausea, upper respiratory mucosal irritation, etc. (18). These symptoms are not related to allergies, and most occur in buildings with a confined space, closed windows, good insulation, and central air conditioning system. The symptoms reduced, or even disappeared, when people are away from the building. In addition, a survey conducted by the National Institute for Occupational Safety and Health, using 2,435 questionnaires to analyze 80 poorly designed buildings in order to understand the effects on the human body, from sensory irritation symptoms (eye fatigue and pain irritation) to general symptoms (headache, fatigue), discovered that SBS has a greater influence on females (30–37%) than males (11–23%) (19). In a set of studies of the associations between questionnaire symptom reports, a study analyzed 160 buildings, and observed that low outdoor airflow rate and presence of certain pollution sources, such as copying machines, tended to be associated with an elevated prevalence of SBS. The SBS presented as more than one general symptom, one mucosal irritation symptom, and one skin symptom occurred weekly, and also affected females (29.6%) more than males (19.8%) (20). Therefore, if the office’s concentration of CO2 is too high, the employees’ work efficiency will be significantly reduced. Air ventilation of office environment might be considered in any building plan to reduce indoor air-related symptoms (19). In addition to some dust, the ER has a propensity to produce not only air pollution, but also a high concentration of CO2, in view of the high density of population.
There were fewer large volatile organic compounds (VOCs) in the triage station, research office and the corridors, while other areas exceeded 150 ppb, due to medical treatment activities. It means that the large VOCs were generated during the medical implementation in a confined space, easily leading to respiratory diseases of the medical personnel in the future. Therefore, medical staff working in the ED should regularly receive chest X-rays to detect potential lung problems early. There are quite variety types of VOCs, and hundreds of organic substances have been tested in the studies of general indoor environments. Concentration of VOCs in new buildings was much greater, often by an order of magnitude or more, and appeared to arise from construction materials and building contents (21,22). Most of them are irritating to the skin or respiratory tract, while others have effects on the central nervous system, causing symptoms such as dizziness and fatigue. Other symptoms could also result from some of them, and yet more substances have been confirmed as carcinogens (23).
Formaldehyde is the most common fugitive contaminant in indoor VOCs (24). It is associated with SBS. Formaldehyde may play a role as the irritant of the nasal mucosa by increasing the expressions of adhesion molecules on HMMECs and by enhancing the adhesiveness between HMMECs and eosinophils (25). Another study indicated that exposure to chemical emissions from indoor formaldehyde was related to asthma, and that some VOCs may cause inflammatory reactions in the airways (26). Our study revealed that, compared to other areas, there was slightly higher formaldehyde concentration (>0.12) around the nursing station the observation room and the research office, which belong to the old building, where the problem of pipeline leakage sometimes occurs. It may be caused by formaldehyde in the solvent or adhesive used by the construction manufacturer.
Indoor ozone (O3) is mainly produced by the use of ultraviolet light and air ionization, so photocopiers and laser printers are the main sources of ozone. The hypothesis was further confirmed by the observation of the correlations among VOCs, ozone, and particles concentrations during a print job with measurable ozone emissions (27). Ozone is an intrinsically toxic gas that is extremely irritating to the eyes and respiratory tract, causing symptoms such as coughing and chest discomfort, and other symptoms. Recent epidemiologic and animal inhalation studies suggest that current ambient levels of ozone are sufficient to cause premature aging of the lungs, although the effects of long-term chronic exposure to ozone remain poorly defined (28). Moreover, symptoms may be aggravated by the stimulation of ozone, for sensitive groups of people such as asthma and respiratory diseases. A study showed that short-term exposure to ozone can increase bronchial allergen responsiveness in subjects with mild allergic asthma or rhinitis (28). With the implementation of computerized physician order entry, the objective called for on-demand barcode printing in a wide variety of settings. In the department of emergency medicine that we studied, more than 20 printers are in operation around the medical staff; however, the space is too small to maintain a proper distance between personnel and printers, meaning that the staffs will inevitably come into contact with ozone. Although the measured concentration of ozone was not high, the measurements might have been affected as a result of the character of ozone, which exists in a very unstable and reactive state that readily and naturally decomposes to oxygen. Concentration of ozone was not easy to accumulate. In the present study, higher concentration of ozone was measured in the research office and the nursing station of the observation room, as a result of the high demand for relevant printers.
Suspended particles have different effects on the respiratory tract depending on their particle size. Generally, PM with a particle size of 10 µm or less are called respirable suspended particulates, or PM10, which can enter the respiratory system with respiration. According to their particle size, it settles in the nasal cavity, respiratory tract and alveolar cells from large to small, and is hazardous to the respiratory tract. Concentrations of PM10 are positively associated with increased numbers of admissions for respiratory diseases (29). The sources of respirable suspended particulates in indoor environments are smoking, cooking, asbestos in synthetic materials, artificial mineral fibers, plant pollen, animal allergens, microbial bacteria, fungi, viruses, and etc. (30). These are harmful to humans in different ways, depending on their characteristics. The survival of aerosolized pathogens depends upon environmental conditions, such as indoor building environment. After all, the worse the ventilation of the hospital is, the longer the same aerosol particles are suspended in the air, the higher the dose of health personnel inhaling the pathogen per unit time, and the higher the chance of infection (31). In the present study, we found the suspended particles level of less than 0.06 mg in the ER, representing that the air conditioning system in the ED of this medical center is qualified in the overall filtration system.
Limitations
This study faced some difficulties, as described below.
A limitation on monitoring locations
In consideration of the medical processing of a large number of emergency patients, we selected monitoring positions that would not affect the patients and medical staffs. Therefore, some of the monitored positions were located on the routes with fewer patients, meaning that the monitoring data obtained might be lower than the actual value. On the other hand, we didn’t setup a measurement control point outside the ER building, due to lack of suitable place. A measurement control point would be more precise and meaningful than global environmental background values, such as the concentration of oxygen (20.9%).
An inadequate monitoring time
The inadequate method-design of this study was the monitoring time, which focused only on three daytime slots. Therefore, fewer statistics data and random area monitoring are both shortcomings. In the future, we should strengthen the analysis of more time periods and spaces, and take it as the basis of assessment in hospital space transforming and planning.
An inadequate data of ER visits
The distribution of ER visits number by time, which allows establishing the relation between time periods and minimum/maximum number of patient visit should be collected. There should be inverse correlation between personnel density and air quality.
The impact of weather
The data of weather as a potential impact factor should be collected, which may affect some results like O3 and PM10 (32).
Conclusions
The ER is a high-risk and harsh environment where it is easy to generate air pollution, as well as a high concentration of CO2. Therefore, maintaining emergency environment and improving air conditioning is a very important issue.
The ventilation of outdoor airflow and filtration of particles of air conditioning systems should be well-designed since the initial construction of ER building to avoid SBS. Current environmental requirements for air conditioning systems are from the beginning to lower the temperature, and later to control the indoor temperature at a comfortable temperature, to the point that it requires a healthy and clean air function. Today’s emergency environment is harmful to the health of medical personnel, because the accumulation of carbon dioxide in some medical treatment spaces can easily lead to fatigue and hypoxia for long-term work of medical staff. Therefore, it is relatively important to improve the air quality, and create a friendly and healthy environment, as well as optimize the air conditioning system functions, so that let the medical staff work with peace of mind.
Future directions
In order to maintain a high-quality healthcare environment in the workplace, a new type of air conditioning system, applied in hospitals and medical facilities, could combine with gas adsorption equipment and nano-photocatalyst air purification technology, to enhance the safe and comfort of working staffs. As a result, the next objective of this study is to develop ideal aerobic air conditioning equipment and modularity in the system, which will maintain the average level concentration of oxygen and reduce the concentration of CO2. Air purification would use titanium dioxide (TiO2) as a catalyst, as it can perform its function even under weak light source, such as an indoor fluorescent lamp. In theory, TiO2 is self-cleaning and pollutant-degrading, so it can purify all types of harmful gases at any time to keep the surrounding air fresh and healthy. Compared with conventional air purification methods (such as physical adsorption method, ultraviolet fixation method, and ozone decomposition method), photocatalyst has the characteristics of simple equipment, strong purifying ability, a wide application range, a long-lasting and effect, no secondary pollution, and low maintenance cost. It can be used for medical areas with major pollution.
In addition, the air conditioning can be combined with real-time monitoring of CO2 concentration, using a computer to calculate the optimal exchange rate of external air, so that it would become an immediate response system, not only providing clean and comfortable air, but also protecting the medical staffs from hazardous substances. At the same time, it can meet the needs of energy saving. In the 21st century, we expect greater artificial intelligence and more energy saving. The statistics show that the air conditioning system accounts for about 40% to 50% of the electricity consumption of medical centers. Consequently, it is necessary to establish an air conditioning trend toward clean air and energy-saving, in order to meet future expectations.
Acknowledgments
The author acknowledges the assistance of the experimental team of Prof. Ching-Song Jwo, a member of the National Taipei University of Technology, in making the project run smoothly.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ht.2019.03.01). WHC serves as an Editor-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Smith KR, Levy BS, Binger A, et al. Development, health, and the environmental risk transition, Ch. 3. International Perspectives in Environment, Development, and Health. New York: Springer, 1997:51-62.
- Dominici F, Bell ML, Pham L, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295:1127-34. [Crossref] [PubMed]
- Seaton A, Godden D, MacNee W, et al. Particulate air pollution and acute health effects. Lancet 1995;345:176-8. [Crossref] [PubMed]
- Wyon DP. The effects of indoor air quality on performance and productivity. Indoor Air 2004;14:92-101. [Crossref] [PubMed]
- Wargocki P, Wyon DP, Baik YK, et al. Perceived Air Quality, Sick Building Syndrome (SBS) Symptoms and Productivity in an Office with Two Different Pollution Loads. Indoor Air 1999;9:165-79. [Crossref] [PubMed]
- Weisel CP, Zhang J, Turpin BJ, et al. Relationship of Indoor, Outdoor and Personal Air (RIOPA) study: study design, methods and quality assurance/control results. J Expo Anal Environ Epidemiol 2005;15:123. [Crossref] [PubMed]
- Pekey B, Bozkurt ZB, Pekey H, et al. Indoor/outdoor concentrations and elemental composition of PM10/PM2.5 in urban/industrial areas of Kocaeli City, Turkey. Indoor Air 2010;20:112-25. [Crossref] [PubMed]
- Baránková P, Naydenov KG, Melikov AK, et al. editors. Distribution of carbon dioxide produced by people in a room: Part 1-Laboratory study. 9th International Conference on Air Distribution in Rooms. 2004: University of Coimbra.
- Bulińska A, Popiołek Z, Buliński ZJB, et al. Experimentally validated CFD analysis on sampling region determination of average indoor carbon dioxide concentration in occupied space. Building and Environment 2014;72:319-31. [Crossref]
- Owen MK, Ensor DS, Sparks LE. Airborne particle sizes and sources found in indoor air. Atmospheric Environment Part A General Topics 1992;26:2149-62. [Crossref]
- Nazaroff WW. Indoor particle dynamics. Indoor Air 2004;14:175-83. [Crossref] [PubMed]
- Organization WH. Practical guidelines for infection control in health care facilities. Manila: WHO Regional Office for the Western Pacific, 2004.
- Moriske HJ, Drews M, Ebert G, et al. Indoor air pollution by different heating systems: coal burning, open fireplace and central heating. Toxicology Letters 1996;88:349-54. [Crossref] [PubMed]
- Turanjanin V, Vučićević B, Jovanović M, et al. Indoor CO2 measurements in Serbian schools and ventilation rate calculation. Energy 2014;77:290-6. [Crossref]
- Vehviläinen T, Lindholm H, Rintamäki H, et al. High indoor CO2 concentrations in an office environment increases the transcutaneous CO2 level and sleepiness during cognitive work. J Occup Environ Hyg 2016;13:19-29. [Crossref] [PubMed]
- Satish U, Mendell MJ, Shekhar K, et al. Is CO(2) an Indoor Pollutant? Direct Effects of Low-to-Moderate CO(2) Concentrations on Human Decision-Making Performance. Environmental Health Perspectives 2012;120:1671-7. [Crossref] [PubMed]
- Redlich CA, Sparer J, Cullen MR. Sick-building syndrome. Lancet 1997;349:1013-6. [Crossref] [PubMed]
- Burge PS. Sick building syndrome. Occupational and Environmental Medicine 2004;61:185. [Crossref] [PubMed]
- Sieber WK, Stayner LT, Malkin R, et al. The National Institute for Occupational Safety and Health Indoor Environmental Evaluation Experience. Part Three: Associations between Environmental Factors and Self-Reported Health Conditions. Applied Occupational and Environmental Hygiene 1996;11:1387-92. [Crossref]
- Sundell J, Lindvall T, Stenberg B, et al. Sick Building Syndrome (SBS) in Office Workers and Facial Skin Symptoms among VDT-Workers in Relation to Building and Room Characteristics: Two Case-Referent Studies. Indoor Air 1994;4:83-94. [Crossref]
- Brown SK, Sim MR, Abramson MJ, et al. Concentrations of Volatile Organic Compounds in Indoor Air – A Review. Indoor Air 1994;4:123-34. [Crossref]
- Brown SK. Volatile organic pollutants in new and established buildings in Melbourne, Australia. Indoor Air 2002;12:55-63. [Crossref] [PubMed]
- Guo H, Lee SC, Chan LY, et al. Risk assessment of exposure to volatile organic compounds in different indoor environments. Environmental Research 2004;94:57-66. [Crossref] [PubMed]
- Kawamura K, Kerman K, Fujihara M, et al. Development of a novel hand-held formaldehyde gas sensor for the rapid detection of sick building syndrome. Sensors and Actuators B: Chemical 2005;105:495-501. [Crossref]
- Kim WJ, Terada N, Nomura T, et al. Effect of formaldehyde on the expression of adhesion molecules in nasal microvascular endothelial cells: the role of formaldehyde in the pathogenesis of sick building syndrome. Clin Exp Allergy 2002;32:287-95. [Crossref] [PubMed]
- Wieslander G, Norbäck D, Björnsson E, et al. Asthma and the indoor environment: the significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int Arch Occup Environ Health 1997;69:115-24. [Crossref] [PubMed]
- Wang H, He C, Morawska L, et al. Ozone-Initiated Particle Formation, Particle Aging, and Precursors in a Laser Printer. Environ Sci Technol 2012;46:704-12. [Crossref] [PubMed]
- Jörres R, Nowak D, Magnussen H. The effect of ozone exposure on allergen responsiveness in subjects with asthma or rhinitis. Am J Respir Crit Care Med 1996;153:56-64. [Crossref] [PubMed]
- Atkinson RW, Ross Anderson H, Sunyer J, et al. Acute Effects of Particulate Air Pollution on Respiratory Admissions. Am J Respir Crit Care Med 2001;164:1860-6. [Crossref] [PubMed]
- He C, Morawska L, Hitchins J, et al. Contribution from indoor sources to particle number and mass concentrations in residential houses. Atmospheric Environment 2004;38:3405-15. [Crossref]
- Tang JW, Li Y, Eames I, et al. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J Hosp Infect 2006;64:100-14. [Crossref] [PubMed]
- Demuzere M, Trigo RM, Vila-Guerau de Arellano J, et al. The impact of weather and atmospheric circulation on O3 and PM10 levels at a rural mid-latitude site. Atmos Chem Phys 2009;9:2695-714. [Crossref]
Cite this article as: Chen PY, Kung LC, Tsai W, Chien DK, Chang WH. The potential risk of sick building syndrome of the emergency department areas in a medical center in Taiwan. Health Technol 2019;3:3.