
The ED length of stay in gunshot injuries: experience in a metropolitan medical center
Introduction
Gunshot injuries are usually caused by suicide attempts, fights and robberies (1-3). The mechanism of gunshot injury is complex and depends on a number of factors, such as the type and velocity of the projectile and the firing distance (4-6). Although the wounds may not always be severe bleeding or lacerating, the ballistic trajectory could cause severe burns or chemical damages to vessels, musculoskeletal or other major organs. It may require an aggressive intervention to stop the bleeding. The high mortality rate is accompanied by complications such as sepsis.
According to prohibitive gun licensing laws, the citizens in Taiwan have been restricted from holding firearms. As a result, gun crime in Taiwan is still uncommon, and there are fewer cases of gunshot wounds (GSW) compared to other countries where people can legally possess weapons such as the United States (1,7). Mackay Memorial Hospital is located at Taipei City, surrounded by nightclubs and red-light districts. Due to this unique location, our hospital becomes the first-line medical center managing gunshot victims in northern Taipei. Few research articles have been published regarding this unique situation in Taiwan (8-10). We are motivated to analyze the characteristics and the emergency department (ED) length of stay (LOS) of GSW patients in the trauma center.
Methods
Study design and population
This retrospective study was conducted in the ED of Mackay Memorial Hospital. Mackay Memorial Hospital is a trauma center located in northern Taipei, Taiwan with 2,000 admission beds and an ED annual census of approximately 120,000. The institutional review board approved the study. All consecutive patients 18 years or older who presented to our ED with gunshot injuries from January 2012 to December 2017 were retrospectively enrolled.
After enrollment, the medical charts and of the enrolled patients were examined for epidemiological data, types of guns, causes of injuries (suicide or assaults), and the survival rate, etc. In addition, we also reviewed the patients’ records for the following analyses: (I) wound position and the correlated clinical presentations; (II) the ED LOS of patients receiving emergency surgery for major organ or vascular injuries. This measurement is the interval between time of ED arrival and time of ED departure to the operation room (OR); (III) LOS in intensive care unit (ICU) and acute physiology and chronic health evaluation (APACHE) score.
Trauma team activation (TTA) criteria
- Primary criteria:
- Unstable vital signs, systolic blood pressure <90 mmHg;
- Fall from height >6 meters or 2 floors;
- Gunshot wound to head, neck and trunk;
- Glasgow Coma Scale (GCS) ≤8;
- Penetrating injury in two or more body regions;
- Severe pelvic fractures;
- Ejection from vehicle;
- Secondary criteria:
- High voltage injury, judged by emergency physician;
- Emergency physician discretion.
Statistical analysis
Descriptive results were reported as mean ± SD when appropriate. Fisher exact test was applied for categorical data in the injury and outcome analysis. Mann-Whitney U test was used for numerical data in the ED LOS analysis. All statistical analyses were completed with SPSS 19.0 version software SPSS (Armonk, NY, USA). Differences were considered to be statistically significant when two-tailed P<0.05.
Results
A total of 27 cases of GSW were collected. A proportion of 74.1% of patients were young age between 20 and 44 years old. The incidence rate was relatively lower (3.7%) in the elder people older than 65 years old. There was only one female patient, and the remaining 26 patients were male. Most of the injuries (81.5%) were intentional attacks and 88.9% of these victims were assaulted by pistols (Table 1).
Table 1
| Variable | N (%) |
|---|---|
| Age, years | |
| 20–44 | 20 (74.1) |
| 45–65 | 6 (22.2) |
| >65 | 1 (3.7) |
| Gender | |
| Male | 26 (96.3) |
| Female | 1 (3.7) |
| Type of injury | |
| Unintentional | 3 (11.1) |
| Assault | 22 (81.5) |
| Suicide | 2 (7.4) |
| Type of weapon | |
| Pistol | 24 (88.9) |
| Stray bullet | 3 (11.1) |
In Table 2, we found the most common injured site was in the extremities (55.6%). Among these 27 patients, 14 patients were with Injury Severity Score (ISS) less than 9 scores, 5 patients between 9 to 15 scores and 8 patients more than 15 scores. Except the 4 out-of-hospital cardiac arrest (OHCA) patients, all the other 23 patients were prescribed antibiotics, including 17 with intravenous form and 6 with oral form. There was no sepsis occurred in these patients during hospitalization. However, 1 patient revisited our hospital 12 days later for intra-abdomen abscess formation.
Table 2
| Clinical characteristic | Result, n (%) | P value* |
|---|---|---|
| Injury site | 0.003 | |
| Head/neck | 6 (22.2) | |
| Chest/upper back | 3 (11.1) | |
| Abdomen/pelvis/lower back | 3 (11.1) | |
| Extremity | 15 (55.6) | |
| Triage | 0.01 | |
| Level I, resuscitation | 10 (37.0) | |
| Level II, emergent | 14 (51.9) | |
| Level III, urgent | 1 (3.7) | |
| Lever IV, less urgent | 2 (7.4) | |
| ISS score | 0.001 | |
| >15 | 8 (29.6) | |
| 9–15 | 5 (18.5) | |
| <9 | 14 (51.9) | |
| Disposition | <0.001 | |
| Death on arrival | 4 (14.8) | |
| Discharge | 6 (22.2) | |
| Ward | 11 (40.7) | |
| ICU | 6 (22.2) | |
| Surgery | 13 (48.1) | 0.134 |
| Trauma team activation | 6 (22.2) | 1.000 |
| Prescribed with antibiotics | – | |
| Intravenous | 17 (63.0) | |
| Oral | 6 (22.2) | |
| Intra-abdominal abscess | 1 (3.7) | – |
| Sepsis | 0 (0) | – |
*, the relationship between mortality and other variables.
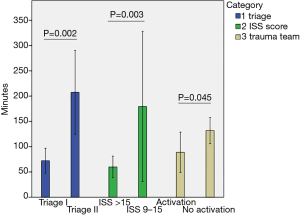
With regards to the ED LOS, the average time in 10 patients with triage I showed statistically significant decline compared to 14 patients with triage II (72.2±34.5 vs. 207.4±143.9 mins, P=0.002). There was a shorter ED LOS of 8 patients with ISS more than 15 comparing to 5 patients whose ISS score were between 9 to 15 (59.9±25.6 vs. 179.4±119.8 minutes, P=0.003). Among these 27 patients, 13 patients had emergency surgery and their average ED stay time was 131.9±31.2 minutes. Even more, the average ED stay time could be shortened to 88.8±32.3 minutes in the 5 patients with TTA (P=0.045) (Figure 1).
As for disposition, 4 OHCA patients had futile resuscitation, including 2 patients shot in the head and 2 patients with multiple gunshot wounds, and 6 patients were not hospitalized due to superficial and minor injuries. The average time of hospital stay of the remaining 17 patients, including 11 in general ward and 6 in ICU, was 9.1±6.9 days. Only one patient passed away in the ICU for severe head injury and all other 16 patients survived. Among the 6 ICU patients, their average duration of ICU stay was 6.2±3.5 days and the average APACHE score was 7.6±4.2. A patient shot in the head had the longest hospital stay of 28 days (Table 2).
Discussion
Our results were in line with others that males (96.3%) were injured by guns more often than females (3.7%) in all age groups (2,11-13). The majority of our GSW injuries were also in younger males (74.1%) (1,11,12). Only 1 male was older than 65 years of age. In addition, our hospital is located in an area with dense civilian population, where low-velocity wounds caused by handguns with projectiles’ muzzle velocity of less than 600 meter per second (m/s) are more common (4). The majority (88.9%) of our cases were injured by pistols, respectively. In addition, most of our patients were victims of assault (81.5%) and only 2 patients were with suicide attempts. The prevalence of our suicidal gunshot injuries (7.4%) was relatively lower than other countries (1,3). Although suicidal gunshot injuries have been clearly associated with poor outcome (5,13-15), one of our patient shot himself and the bullet only got stuck at his temporal subcutaneous region without penetrating into the skull. This might be because guns are not easily obtained by our civilians. They may be unfamiliar with the way of shooting or use the handmade pistols.
In the literature, it has been pointed out that the mortality rate of GSW in the brain is related to GCS (8,14-16). In our study, there were only 6 patients with GSW in the head. Among them, 4 cases (66.7%) were dead, including 3 cases of OHCA and 1 case of in-hospital cardiac arrest (IHCA). The mortality rate was similar to 51–84% reported by previous studies (8,15,16). The GCS of the case of IHCA was E1M2V1 with dilated pupils on both sides and without light reflex while sent to the ED. This patient did not receive surgical treatment and expired at the ICU 4 days after admission. We found that if the ballistic damage patients have a GCS of less than 4, the mortality rate is 100% in our subjects. The mortality of injury in the head is significantly higher than other organs.
We further analyzed the ED LOS in different groups of triage level and ISS score. The study results suggest that the important factor affecting ED LOS during such an incident is waiting for operation once a disposition decision has been made. The reasons for the increasing output time interval might be due to an inadequate number of surgeon and operating rooms for emergent trauma patients. For the 13 surgical patients, 5 triage level I cases whose ISS scores were between 9 to 25 were treated by an activated trauma team, and their ED LOS could be diminished to the shortest. From a time-effectiveness perspective, our study identified that a trauma team response might initially improve the quality of patient care in severe GSW injuries by shortening the time from arrival in the ED to assessment and management (17,18). Consistent with growing evidence, patients treated by trauma teams have been shown to have shorter ED stay time, ED to computed tomographic imaging time and ED to OR time (19-21), which can further save lives and prevent long-term disability (19,22,23).
We acknowledge that there are some limitations in our study. Owing to the retrospective design with its inherent selection bias lacks the data on the circumstances of the mechanisms of injury and the appearance of wounds. On the other hand, the small sample size conducted at a single urban trauma center in northern Taiwan, which may not be representative of other populations. In addition, there might be unmeasured confounders, such as time interval of waiting for ED registration, and man-made factors of time records. However, the authors did make every attempt to collect all data from a computer database and medical records. All enrolled patients had precise data for each variable, with no missing data.
Conclusions
TTA in severe GSW patients indeed shorten the ED LOS and might initially improve the quality of patient care. This is the result of better trauma systems, including advances in care from emergency medical services and the acute care surgical management.
Acknowledgments
We express gratitude to Yen-Kuang Lin, Research Fellow, Biostatistics Center, Taipei Medical University, Taipei, Taiwan to help our statistical analysis.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ht.2019.01.01). WHC serves as an Editors-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the MacKay Memorial Hospital Institutional Review Board (No. 18MMHIS045e) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Naghavi M, Marczak LB, Kutz M, et al. Global Mortality From Firearms, 1990-2016. JAMA 2018;320:792-814. [Crossref] [PubMed]
- Backman PB, Riddez L, Adamsson L, et al. Epidemiology of firearm injuries in a Scandinavian trauma center. Eur J Trauma Emerg Surg 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Cook A, Osler T, Hosmer D, et al. Gunshot wounds resulting in hospitalization in the United States: 2004-2013. Injury 2017;48:621-7. [Crossref] [PubMed]
- Lichte P, Oberbeck R, Binnebösel M, et al. A civilian perspective on ballistic trauma and gunshot injuries. Scand J Trauma Resusc Emerg Med 2010;18:35. [Crossref] [PubMed]
- Rajasingh CM, Tennakoon L, Staudenmayer KL. Self-inflicted gunshot wounds: readmission patterns. J Surg Res 2018;223:22-8. [Crossref] [PubMed]
- Stevenson T, Carr DJ, Penn-Barwell JG, et al. The burden of gunshot wounding of UK military personnel in Iraq and Afghanistan from 2003-14. Injury 2018;49:1064-9. [Crossref] [PubMed]
- Mann JJ, Michel CA. Prevention of Firearm Suicide in the United States: What Works and What Is Possible. Am J Psychiatry 2016;173:969-79. [Crossref] [PubMed]
- Tsuei YS, Sun MH, Lee HD, et al. Civilian gunshot wounds to the brain. J Chin Med Assoc 2005;68:126-30. [Crossref] [PubMed]
- Wu CC, Young YH. Ten-year longitudinal study of the effect of impulse noise exposure from gunshot on inner ear function. Int J Audiol 2009;48:655-60. [Crossref] [PubMed]
- Chuang TY, Chiou-Tan FY, Vennix MJ. Brachial plexopathy in gunshot wounds and motor vehicle accidents: comparison of electrophysiologic findings. Arch Phys Med Rehabil 1998;79:201-4. [Crossref] [PubMed]
- Norton J, Whittaker G, Kennedy DS, et al. Shooting up? Analysis of 182 gunshot injuries presenting to a London major trauma centre over a seven-year period. Ann R Coll Surg Engl 2018;100:464-74. [Crossref] [PubMed]
- Fitzpatrick V, Castro M, Jacobs J, et al. Nonfatal Firearm Violence Trends on the Westside of Chicago Between 2005 and 2016. J Community Health 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Bertisch H, Krellman JW, Bergquist TF, et al. Characteristics of Firearm Brain Injury Survivors in the Traumatic Brain Injury Model Systems (TBIMS) National Database: A Comparison of Assault and Self-Inflicted Injury Survivors. Arch Phys Med Rehabil 2017;98:2288-94. [Crossref] [PubMed]
- Maragkos GA, Papavassiliou E, Stippler M, et al. Civilian Gunshot Wounds to the Head: Prognostic Factors Affecting Mortality: Meta-Analysis of 1774 Patients. J Neurotrauma 2018;35:2605-14. [Crossref] [PubMed]
- Deng H, Yue JK, Winkler EA, et al. Adult Firearm-Related Traumatic Brain Injury in United States Trauma Centers. J Neurotrauma 2019;36:322-37. [Crossref] [PubMed]
- Glapa M, Zorio M, Snyckers FD, et al. Gunshot wounds to the head in civilian practice. Am Surg 2009;75:223-6. [PubMed]
- Hsu CM, Liang LL, Chang YT, et al. Emergency department overcrowding: Quality improvement in a Taiwan Medical Center. J Formos Med Assoc 2019;118:186-93. [Crossref] [PubMed]
- Chen SY, Chaou CH, Ng CJ, et al. Factors associated with ED length of stay during a mass casualty incident. Am J Emerg Med 2016;34:1462-6. [Crossref] [PubMed]
- Cameron PA, Gabbe BJ, Smith K, et al. Triaging the right patient to the right place in the shortest time. Br J Anaesth 2014;113:226-33. [Crossref] [PubMed]
- Cohen MM, Fath JA, Chung RS, et al. Impact of a dedicated trauma service on the quality and cost of care provided to injured patients at an urban teaching hospital. J Trauma 1999;46:1114-9. [Crossref] [PubMed]
- Liberman M, Mulder DS, Jurkovich GJ, et al. The association between trauma system and trauma center components and outcome in a mature regionalized trauma system. Surgery 2005;137:647-58. [Crossref] [PubMed]
- Jurkovich GJ. Regionalized health care and the trauma system model. J Am Coll Surg 2012;215:1-11. [Crossref] [PubMed]
- Lendrum RA, Lockey DJ. Trauma system development. Anaesthesia 2013;68:30-9. [Crossref] [PubMed]
Cite this article as: Liu LR, Chen CC, Lai JI, Chiu YH, Chang WH. The ED length of stay in gunshot injuries: experience in a metropolitan medical center. Health Technol 2019;3:1.


